Motilent Monthly Digest #12
Motilent in October ✈️ UEG ✈️ ACG | A summer of 21 abstracts | Gastroparesis Awareness Month
🗞 News
✈️ Motilent are gearing up for UEG and ACG in October - Click to book a meeting on calendly: UEG / ACG or drop us an email at info@motilent.io
😎 21 abstracts have been released over the summer across 5 conferences - see below which ones made our top 3
🤔 “We should scrap the name Gastroparesis” - Alex took to Linkedin to share his thoughts on Gastroparesis awareness month
👁 ⬇️ Look at this!
Motilent’s been on the road this summer! Its been great to see so many of you on the floor. Thank you all for your support and high quality work.
SPR ➡️ SAR ➡️ DDW ➡️ ESGAR ➡️ ASCRS
….and if you haven’t caught us at a conference yet this year we’ll be at ACG, UEG and RSNA later this year!
☀️😎 A Summer of Abstracts
Here’s our top 3:
….all others listed below👇
1. Dynamic magnetic resonance imaging reveals that post-operative ileus is associated with hyperactive distal colonic motility Chapman et al. (Leeds, UK)
Summary: At least half the ileus patients seem to have too much colonic contractility. Maybe we should be looking for ways to identify this group then calm the bowel down?
2. Volumetric Assessment of Treatment Response in Newly Diagnosed Crohn Disease: A Pilot Study Derinkuyu et. al. (Cincinnati, US)
Summary: What’s better than bowel wall thickness? Bowel wall volume! Or so it would seem in kids with Crohn’s Disease. Presented at SAR. Changes shown as early as 8 weeks with greater dynamic range than BWT alone.
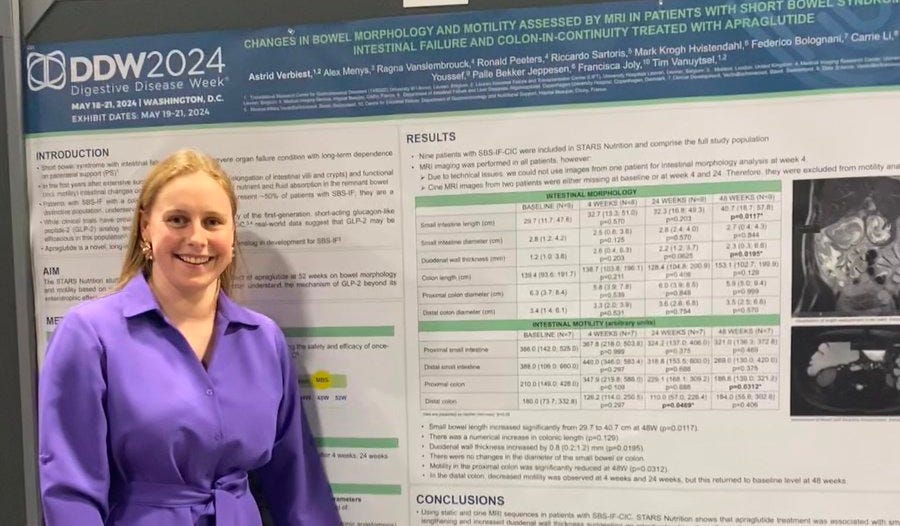
3. CHANGES IN BOWEL MORPHOLOGY AND MOTILITY ASSESSED BY MRI IN PATIENTS WITH SHORT BOWEL SYNDROME INTESTINAL FAILURE (SBS-IF) AND COLON-IN-CONTINUITY (CIC) TREATED WITH APRAGLUTIDE Verbiest* et al. (KU Leuven)
Summary: We’ve heard about GLP-1 but what about GLP-2? Here we saw this class of drug broadly reducing pan-gut contractility in a small, but thorough, pilot in patients with Short Bowel Syndrome. Less contractions, more absorption, better nutrition?
*pictured below at DDW
August was Gastroparesis awareness Month!
Here is a summary from Alex:
Gastroparesis - the chronic feeling of bloating, nausea and upper GI discomfort. With GLP1 helping to boost the prevalence to 1-2% of the population, is it finally getting the attention it deserves?
Let’s take a closer look for Gastroparesis awareness month. The stomach is a complex system that senses, stretches and breaks down our food chemically and mechanically. It carefully expands to ‘accommodate our meal’ before stretch receptors say ‘stop we’re full!’ It’ll signal to the small bowel and colon while communicating back and forth with the brain. It’s all got to work correctly.
Imagine an orchestra, all the players need to be doing their part for the performance to sound right. One rogue tuba and you have a farce on your hands. But how can you identify the wrong thing happening if you’re watching the performance on the TV with the sound off?
Here are my key takeaways for gastroparesis awareness month, we need:
📈 Better, holistic testing of gut health - The central dogma of gastroparesis is the presence of ‘delayed gastric emptying’ basically the only thing we can measure routinely in clinic. High inter-patient variability, (gastroparesis one week, functional dyspepsia the next and inseparable from a healthy control a month later) is one of the major challenges we need to overcome. A battery of tests measuring accommodation, contractility, pyloric function etc is almost certainly needed to phenotype patients. At the moment, we’re watching that person with the gong in the percussion section.
🎯 Objective trial endpoints - the FDA have recently dropped our one test, gastric emptying, as a primary and secondary endpoint moving entirely towards patient reported outcomes (PRO). Symptoms are crucial but without knowing what’s driving, for example, ‘fullness,’ patient selection and proof of efficacy is extremely challenging.
🧘 Treat the patient not the symptoms: The brain and gut-brain axis have probably as much to do with symptoms as the gut itself. We need more input from allied specialties (e.g psychology and psychiatry) to complement gastric tests and support PRO development. If the orchestra’s not watching the conductor, they can end up playing the wrong concerto beautifully.
There are few quick wins in modern medicine. Most of our healthcare burden today lies in complex, chronic diseases that lie outside of any one specialty. My orchestra metaphor is now stretched thin but we’re not looking at ‘solos’ anymore, we’re watching at the whole performance. We should scrap the name Gastroparesis, share ideas openly and be willing to go back to the start where necessary to enable science based management of what we should start calling ‘disorders of gastric physiology.’
🔗 From socials
Let's talk standardisation of MRE Reporting in IBD. Everyone does the same thing right….? 😳👇
Apparently not! The burden of Inflammatory Bowel Disease (IBD) is rising with a prevalence of 1 in every 200-300 people in Europe and the US highlighted in a recent high-impact piece from the BBC News and Crohn's & Colitis UK. Standardising MRI reports is essential for detecting complications, monitoring therapeutic response, and predicting long-term outcomes.
In a recent study Luca Balzarini et al surveyed 253 radiologists across Italy in April 2023 on their experiences with Magnetic Resonance Enterography (MRE) in IBD cases.
Abstracts links:
Thank you all for using our tech to answer a range of fascinating and important questions between the months of April and June. If anyone wants putting in touch with anyone else please reach out.
MRI gastric motility assessment in patients with upper gastrointestinal symptoms using a spatiotemporal motility mapping tool – a feasibility study Jason Mak, Heather Fitzke, Tianci Hu,Asma Fikree,Natalia Zarate-Lopez & Stuart Taylor
Dynamic magnetic resonance imaging reveals that post-operative ileus is associated with hyperactive distal colonic motility Stephen J. Chapman, Mikolaj Kowal, Jack Helliwell, Iyad Naim, Tom Robbins, Alex Menys, Damian J. Tolan & David G. Jayne
Magnetic Resonance Imaging-Based Average T2 Signal as A Non-Invasive Measure of Fibrosis In Enteric Crohn’s Disease I Naim, C Clarke, C Hoad, N Jinnah, A Mukherjee, P Gowland, O Mougin, A Menys, A Bard, G W Moran
Intestinal Motility Changes in Patients Undergoing Removable Stent Treatment for Focal Crohn’s Disease Strictures R Das, R Singh, A Menys, S Din, C Hoad, J Lund, A Cole
Changes in 3D volumetry of perianal fistulas can predict the clinical outcome in perianal fistulizing Crohn’s disease. I Ordás Jiménez, M.D.- Ph.D, B Caballol, C Saavedra, A Fernández-Clotet, M Masamunt, E Ricart, J Rimola
Volumetric Assessment of Treatment Response in Newly Diagnosed Crohn Disease: A Pilot Study B E Derinkuyu, A Bard, I Naim, J A Tkach, L A Denson, J R Dillman
Changes in 3D volumetry of perianal fistulas can predict the clinical outcome in perianal fistulizing Crohn’s disease. I Ordás Jiménez, M.D.- Ph.D, B Caballol, C Saavedra, A Fernández-Clotet, M Masamunt, E Ricart, J Rimola
Intestinal Motility Changes in Patients Undergoing Removable Stent Treatment for Focal Crohn’s Disease Strictures R Das, R Singh, A Menys, S Din, C Hoad, J Lund, A Cole
Changes in 3D volumetry of perianal fistulas can predict the clinical outcome in perianal fistulizing Crohn’s disease. I Ordás Jiménez, M.D.- Ph.D, B Caballol, C Saavedra, A Fernández-Clotet, M Masamunt, E Ricart, J Rimola
MRI Of Complex Perianal Fistula Interpreted With The Aid Of A Rapid 3d Interactive Model: Initial Experience. G.Bhatnagar, L.Lindsay, L.Carter, I. Niam, K. Williams, J. Huddy
Quantified Motility And Structured Anatomical Scoring In Clinical Practice - A Real World Investigation Of Emerging Markers Of Small Bowel Crohn's Disease Activity G. Bhatnagar, A. Bhagwanani, A. Menys, I. Naim, T. Shepherd, S. Rahman; London/UK
Volumetric Assessment of Treatment Response in Newly Diagnosed Crohn Disease: A Pilot Study B E Derinkuyu, A Bard, I Naim, J A Tkach, L A Denson, J R Dillman
Dynamic magnetic resonance imaging reveals that post-operative ileus is associated with hyperactive distal colonic motility Stephen J. Chapman, Mikolaj Kowal, Jack Helliwell, Iyad Naim, Tom Robbins, Alex Menys, Damian J. Tolan, David G. Jayne
Quantified Motility MR Enterography Response Assessment in Paediatric Inflammatory Bowel Disease Riwa Meshaka,Heather Fitzke,Joy Barber,Kelsey Jones,Stuart Taylor,Tom Watson
MRI-based ileal motility quantification predicts stricture response to biologic therapy in Crohn Crohn's: a pilot study. Valeria Pena Trujillo, MD
Changes in bowel morphology and motility assessed by MRI in patients with short bowel syndrome intestinal failure (SBS-IF) and colon-in-continuity (CIC) treated with apraglutide. A. Verbiest, A. Menys, R. Vanslembrouck, R Peeters, R. Sartoris, M. Hvistendahl, F. Bolognani, C. Li, N. Youssef, P. Jeppesen, F. Joly & T. Vanuystel
METRIC-EF: Magnetic resonance enterography to predict disabling disease in newly diagnosed Crohn’s disease – A multicenter, non-randomised, single arm, prospective study Shankar Kumar,Andrew Plumb,Sue Mallett,Gauraang Bhatnagar, Stuart Bloom, Caroline S Clarke, John Hamlin, Ailsa L Hart, Ilan Jacobs, Simon Travis, Roser Vega, Steve Halligan,Stuart Andrew Taylor
Quantified motility and structured anatomical scoring in clinical practice – A real world investigation of emerging markers of small bowel Crohn’s disease activity. G. Bhatnagar, A. Bhagwanani, A. Menys, I. Naim, T. Shepherd, S. Rahman
Volumetric measurement of terminal ileal Crohn’s disease by MR enterography: A feasibility study Shankar Kumar, Nikhil Rao, Anisha Bhagwanani, Thomas Parry, Maira Hameed, Safi Rahman, Heather E Fitzke, Judith Holmes, Benjamin Barrow, Andrew Bard, Alex Menys, David Bennett, Sue Mallett, Stuart A Taylor
Motility at cine-MRI in stricturing Crohn’s disease patients to evaluate stricture composition. K. Beek, F. van Rijn, C. de Jonge, F. de Voogd, C. Buskens, A. Mookhoek, E. Neefjes-Borst, K. Horsthuis, J. Tielbeek, G. D’Haens, K. Gecse, J. Stoker
The goal here is to bring together a quick round up of interesting content, news and imagery relevant to - and I know this sounds oddly specific - the non-invasive IBD community with occasional forays into the mechanistic elements of diseases featuring GI problems (e.g. Cystic Fibrosis, Parkinson's, gastroparesis etc).
Feedback is very welcome, especially around hot topics in the industry and might even make it into a future newsletter. If there are any community messages that need passing along (jobs, studies, points of interest etc) we’re happy to communicate them here.
And lastly - if you know anyone in the space, please forward this on and encourage them to subscribe.
Alex Menys, CEO & Honorary Associate Prof at UCL